Dr. Shilpa Kshatriya–Perioperative Evaluation of Patients Undergoing Noncardiac Surgery

Shilpa Kshatriya, MD
Recently, the American College of Cardiology and American Heart Association published updated guidelines in 2014 to help provide guidance to physicians on management of patients for noncardiac surgery.
DEFINITIONS:
Emergency procedure— one in which life or limb is threatened if not in the operating room, where there is little or no time for clinical evaluation, typically within < 6 hours.
Urgent procedure– a procedure in which there may be time for a limited clinical evaluation, usually when life or limb is threatened if not in the operating room, typically between 6 and 24 hours.
Time – sensitive procedure– one in which a delay of > 1 to 6 weeks to allow for an evaluation and significant changes in management will negatively outcome, e.g. oncologic procedures
Elective procedure– one in which the procedure could be delayed for up to 1 year.
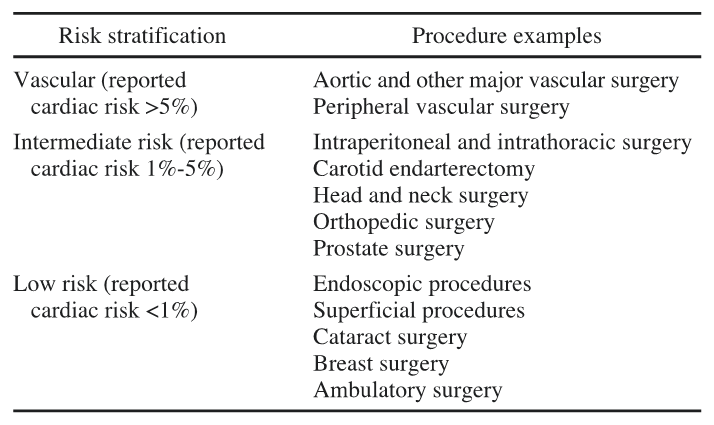
CLASSIFICATION OF RISK:
Low-risk– procedure in which the risk of a major adverse cardiac event (MACE) of death or myocardial infarction (MI) of < 1%, e.g cataract and plastic surgery
Elevated risk– procedures with a risk of MACE ≥ 1 %.
METHODS OF ASSESSING RISK:
Three parameters determine risk of cardiac morbidity and mortality with noncardiac surgery: 1) type of procedure 2) patient’s clinical characteristics 3) functional status
1) SURGICAL RISK:
HIGH RISK (cardiac risk > 5%)- emergency major surgeries, aortic and other major vascular surgeries, peripheral vascular surgery
INTERMEDIATE RISK SURGERY- carotid endarterectomy, intraperitoneal and intrathoracic surgery, head and neck surgery, orthopedic surgery
LOW RISK SURGERY-breast surgery, cataract surgery, endoscopic procedures
2) PATIENT RISK:
REVISED CARDIAC RISK INDEX (RCRI) RISK CALCULATOR:
Lee and coworkers who devised a six-point index score for assessing the risk of complications with noncardiac surgery. The Revised Cardiac Risk Index (RCRI) includes the following variables and risks:
- High-risk surgery (intrathoracic, intra-abdominal. or suprainguinal vascular)
- Ischemic heart disease (defined as a history of MI, pathologic Q waves on the ECG, use of nitrates, abnormal stress test, or chest pain secondary to ischemic causes)
- Congestive heart failure
- History of cerebrovascular disease
- Diabetes requiring insulin therapy
- Preoperative serum creatinine level higher than 2 mg/dL
Each of the six risk factors was assigned one point. Patients with none, one, or two risk factor(s) were assigned to RCRI classes I, II, and III, respectively, and patients with three or more risk factors were considered class IV. The risk associated with each class was 0.4%, 1%, 7%, and 11% for patients in classes I, II, III, and IV, respectively.
HIGH RISK CONDITIONS -FIX THESE CONDITIONS PRE-OP:
Unstable coronary syndromes –unstable angina, recent MI (> 7 days and < 30 days)
Decompensated heart failure
Significant arrhythmias – high-grade AV block (third degree AV block, Mobitz II AV block), symptomatic ventricular arrhythmias, symptomatic bradycardia, supraventricular arrhythmias (including atrial fibrillation) with heart rate > 100
Severe valvular disease- severe aortic stenosis, symptomatic mitral stenosis
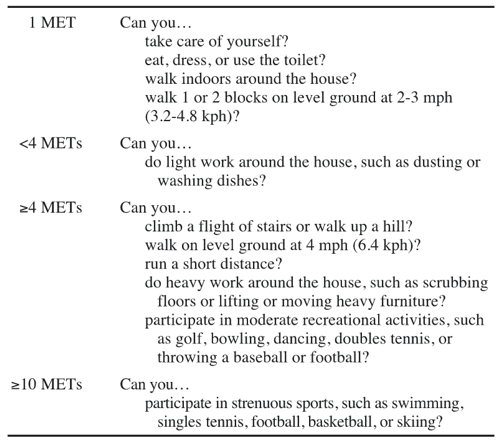
3) FUNCTIONAL CAPACITY:
Perioperative cardiac risk is increased in patients unable to exercise ≥ 4 METS (metabolic equivalents). Functional capacity can be easily assessed in the office. Typical household chores require 1 to 2 METS and climbing 2 flights of stairs or walking more than 4 blocks denote > 4 METS of activity. Further preoperative testing can often be deferred if patients have good functional capacity ≥ 4 METS, in the absence of active cardiac conditions e.g. unstable angina
ENERGY EXPENDITURE FOR VARIOUS ACTIVITIES:
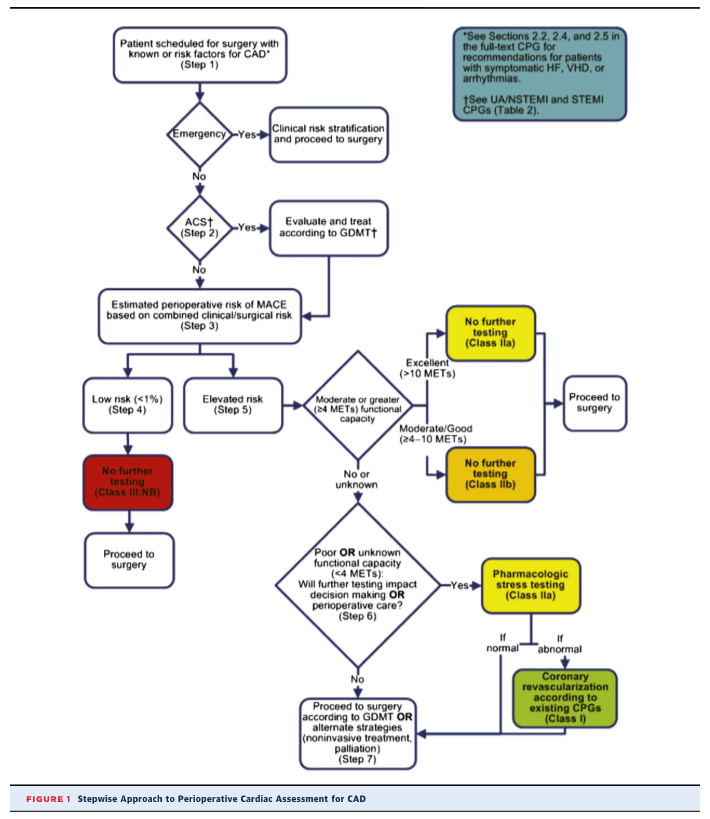
STEP-WISE APPROACH TO PERIOPERATIVE CARDIAC ASSESSMENT:
ROLE OF STRESS TESTING PRIOR TO NONCARDIAC SURGERY:
- For patients with elevated risk and excellent functional capacity (4 to 10 METS or more) it is reasonable to defer exercise testing and proceed to surgery.
- For patients with elevated risk and poor ( < 4 METS) or unknown functional capacity it is reasonable to perform exercise testing with cardiac imaging if it will change management.
- Routine screening with stress testing is not useful for patients at low risk for noncardiac surgery.
ROLE OF PREOP CORONARY ANGIOGRAPHY PRIOR TO NONCARDIAC SURGERY:
Not recommended UNLESS patients are suspected to have unstable coronary disease for which elective noncardiac surgery would have to be delayed.
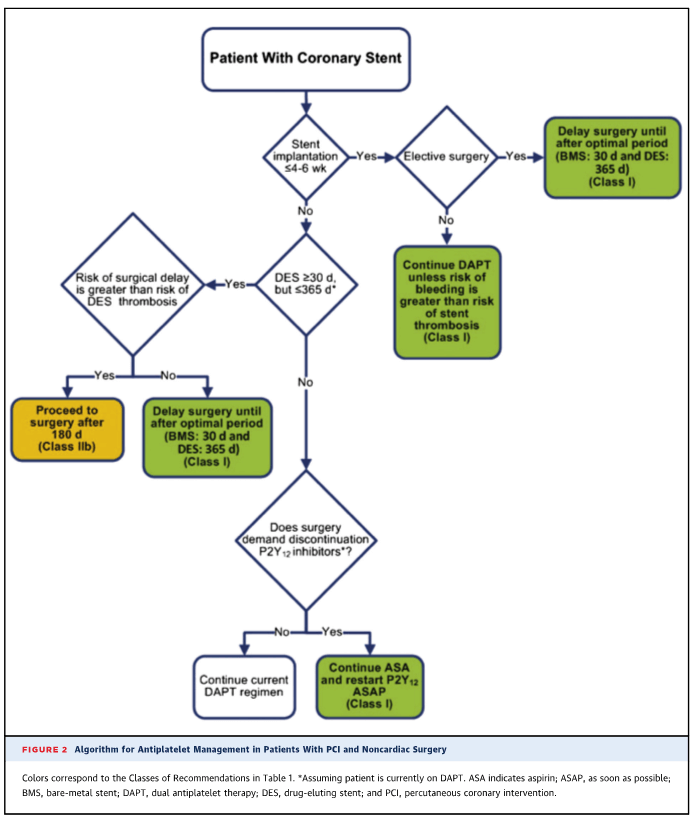
TIMING OF ELECTIVE NONCARDIAC SURGERY IN PATIENTS WITH PRIOR CORONARY INTERVENTION (PCI)
Elective noncardiac surgery should be delayed-
- 14 days after balloon angioplasty
- 30 days after bare metal stent implantation
- 365 days optimallyafter drug-eluting stent implantation
ROLE OF BETA BLOCKERS:
- Beta blocker should be continued in patients undergoing surgery who have been on beta blockers previously
- It is reasonable to start beta blocker in the perioperative period in patients with intermediate or high risk ischemia on stress testing or in those with 3 or more RCRI risk factors (DM, CHF, CAD, CKD, CVA)
- If started prior to surgery it is preferable to start beta blockers more than one day prior to surgery (ideally 2 to 7 days before surgery)
ROLE OF STATINS:
- Statins should be continued in patients already taking statins and scheduled for noncardiac surgery.
- Perioperative initiation of statin use is reasonable in patients undergoing vascular surgery.
ANTIPLATELET MANAGEMENT IN PATIENTS WITH PCI AND NONCARDIAC SURGERY:
Reference:
Fleisher LA, et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am CollCardiol 2014;64:e77–137